[ad_1]
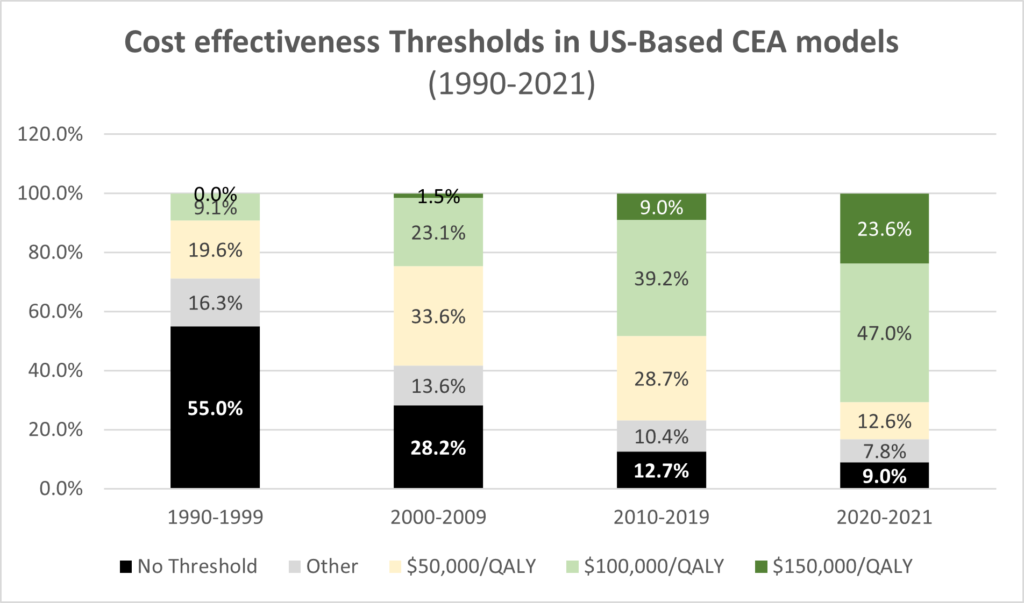
That is the questions Peter Neumann and David Kim (2023) answer in their JAMA research letter published today. They use 1990-2021 data from the Tufts Medical Center CEA Registry. The results are summarized in the graphs below.
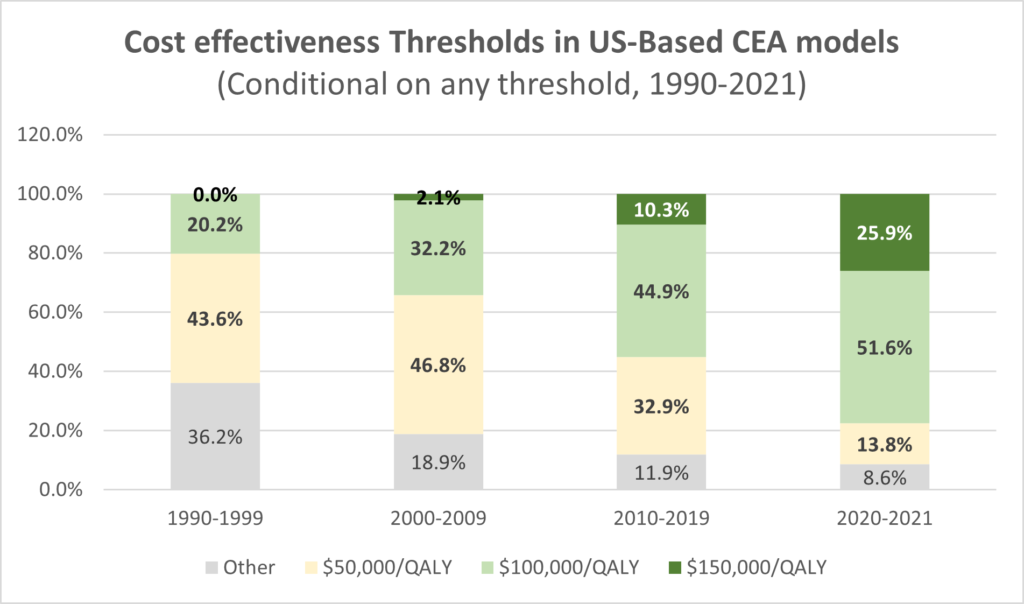
First, we see the use of a explicit cost effectiveness threshold increasing over time, from only 45% of published studies to 91% of all studies. Second, the cost-effectiveness thresholds have increased over time. Whereas 43.6% of studies reporting a CEA threshold used a $50,000/QALY threshold in the 1990s, now only 13.8% of studies use that threshold; whereas 0% of studies used $150,000/QALY threshold in the 1990s, now 25.9% of studies do so.
The authors also note that:
- Cancer-related CEAs referenced higher thresholds than non-cancer CEAs, which may suggest a view that interventions for diseases associated with greater mortality and morbidity warrant higher thresholds.
- Authors of industry-funded analyses tend to reference higher thresholds.
You can read the full paper here.
[ad_2]